Introduction
Alcohol is woven into many cultures, celebrations, and lifestyles around the world — from a glass of wine with dinner to beers shared with friends. But amid its social appeal lies a serious health truth: alcohol consumption is a known risk factor for multiple cancers. Thousands of people worldwide develop cancer each year that’s linked to alcohol intake, whether through heavy drinking or patterns of consumption over decades. In this in-depth guide, we explore:
- How alcohol intake increases cancer risk
- Biological mechanisms behind alcohol-related cancer
- The surprising causes of lung cancer in non-smokers
- Prevention strategies that could help reduce your risk
We also pack this article with SEO-friendly keywords like alcohol and cancer link, alcohol cancer risk, lung cancer causes in non-smokers, ethanol carcinogenic effects, and healthy lifestyle and cancer prevention — so it reaches the people who most need this information.
Alcohol and Cancer: What Research Says
Most people already know that smoking causes cancer. But alcohol’s role in cancer development is less widely understood — even though evidence over decades now confirms it.
1. Alcohol as a Carcinogen
The International Agency for Research on Cancer (IARC) classifies ethanol — the active ingredient in alcoholic beverages — as a Group 1 carcinogen, meaning it definitely causes cancer in humans.
Here’s how alcohol increases cancer risk:
- Ethanol is metabolized into acetaldehyde, a toxic and DNA-damaging chemical.
- Alcohol creates reactive oxygen species (ROS) that damage DNA and promote inflammation.
- It impairs nutrient absorption (like folate), which normally helps protect against cancer.
- Alcohol can increase estrogen levels, linked to breast cancer.
This combination can speed up the transformation of normal cells into cancerous ones.
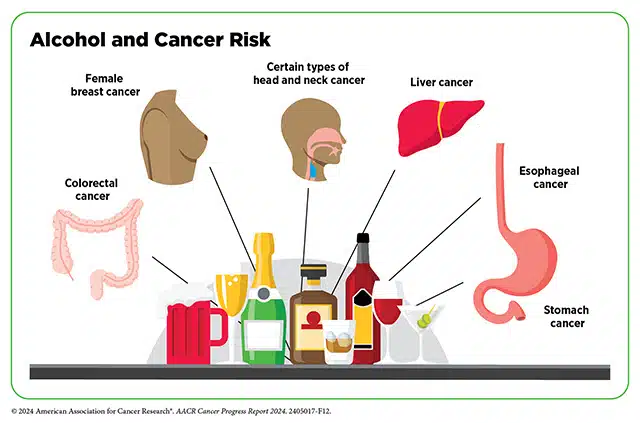
2. Which Cancers Are Linked to Alcohol Intake?
Research shows multiple cancer types are associated with alcohol consumption, including:
✔ Mouth cancer
✔ Pharynx and larynx cancer
✔ Esophageal cancer
✔ Breast cancer
✔ Colorectal cancer
✔ Liver cancer
✔ Stomach cancer
The risk increases with the amount of alcohol consumed, meaning heavier drinking generally carries higher cancer risk.
A notable U.S. Surgeon General report emphasized that even moderate drinking increases the likelihood of several cancers, and risks grow with each drink added per day.
Alcohol Intake and Lung Cancer: What’s the Link?
When it comes to lung cancer, smoking is the dominant risk — but that doesn’t mean other factors don’t matter.
1. Does Alcohol Cause Lung Cancer?
The relationship between alcohol consumption and lung cancer is less direct than it is for other cancer types. Some large studies have noted possible risk increases among heavy drinkers, especially in men and those who also smoke. In fact:
- One pooled analysis found that high alcohol intake (30 g/day or more) was associated with a slightly greater lung cancer risk.
- Among male non-smokers, intense levels of alcohol intake were strongly linked with higher lung cancer risk in certain studies — though these findings may be influenced by other factors.
However, research specifically in non-smokers has been mixed, and some meta-analyses suggest no clear independent connection between alcohol and lung cancer in people who have never smoked.
2. So Why Does it Matter?
Alcohol may contribute indirectly to lung cancer risk in several ways:
- By increasing oxidative stress and inflammation, which can affect many organs.
- By impairing nutrient absorption, weakening the body’s defense against cellular changes.
- By interacting with other environmental toxins, like air pollution or secondhand smoke, especially in non-smokers.
In other words, while alcohol may not independently cause lung cancer in every case, its biological effects can create an environment where cancer is more likely to develop.
Understanding Lung Cancer in Non-Smokers
Lung cancer in people who have never smoked is a critical and growing public health issue. Around 15–20% of lung cancer cases worldwide occur in non-smokers.
And, as recent health reports from cities like Lucknow show, in some populations up to 25–30% of lung cancer patients have never smoked — including women, younger adults, and people exposed to pollution or indoor smoke.
Key Causes of Lung Cancer in Non-Smokers
Here are the main risk factors beyond tobacco:
1. Air Pollution
Fine particulate matter (PM2.5) from traffic, industrial emissions, and biomass fuel use can penetrate deep into the lungs, triggering DNA damage over time.
2. Secondhand Smoke
Living around smokers exposes non-smokers to carcinogenic particles similar to active smoking.
3. Radon Gas Exposure
Radon, a natural radioactive gas in soil and buildings, is a leading cause of lung cancer in non-smokers globally.
4. Occupational Hazards
Asbestos, silica, diesel exhaust, and certain chemicals increase the risk of lung cancer even without smoking.
5. Genetics and Molecular Changes
Inherited or acquired genetic mutations (like EGFR or ALK) can drive lung cancer in non-smokers, particularly in adenocarcinoma — the most common subtype in this group.
6. Lifestyle and Diet
Poor diet, obesity, and lack of physical activity can all play a role in cancer risk by weakening immune defenses and increasing systemic inflammation.
How Alcohol and Lung Cancer Risks Intersect
While alcohol isn’t a primary cause of lung cancer in non-smokers, it may still influence risk in combination with other factors:
- Heavy alcohol intake can worsen immune function, making the lungs less able to control abnormal cells.
- Alcohol can increase susceptibility to oxidative and inflammatory damage from pollutants or infections.
For non-smokers living in high-pollution areas, even small compounding effects matter.
Prevention: How to Reduce Your Cancer Risk
Understanding risk is one thing — acting on it is another. Here are key strategies that research and health experts unanimously recommend:
1. Reduce or Stop Alcohol Consumption
The most effective way to eliminate the cancer risk from alcohol is to avoid or minimize intake. The Cleveland Clinic and other authorities advise limiting alcohol to very low levels — or not at all — to lower cancer risk.
2. Avoid Smoking and Secondhand Smoke
Smoking remains the strongest lung cancer risk factor, so quitting is essential — and protects others too.
3. Reduce Air Pollution Exposure
Use air purifiers, avoid heavy-traffic areas, and support clean air initiatives in your community.
4. Test for Radon
Radon can accumulate indoors — testing and mitigation can dramatically reduce risk.
5. Eat a Balanced, Anti-Inflammatory Diet
High intake of fruits, vegetables, whole grains and omega-3 fats supports cellular repair and reduces inflammation.
6. Get Regular Health Screenings
Early diagnosis improves cancer outcomes drastically.
Final Thoughts
Alcohol intake is more than a social or lifestyle choice — it’s a meaningful cancer risk factor. While the link between alcohol and lung cancer in non-smokers isn’t as direct as with other cancer types, the overall biological effects of alcohol — combined with environmental and genetic factors — make moderation or abstinence a wise choice for health-minded individuals.
Whether you’re here to learn how to protect yourself or to inform others, understanding these connections empowers you to make choices that reduce cancer risk, support long-term health, and promote a healthier tomorrow.
Useful Resources & References
- National Cancer Institute – Alcohol and Cancer Risk: https://www.cancer.gov/about-cancer/causes-prevention/risk/alcohol/alcohol-fact-sheet
- Cleveland Clinic – Cancer Prevention and Alcohol: https://my.clevelandclinic.org/departments/cancer/patient-education/wellness-prevention/cancer-risk-factors
- Lung Cancer Causes (American Cancer Society): https://www.cancer.org/cancer/types/lung-cancer/causes-risks-prevention/what-causes.html
- PubMed research on alcohol and lung cancer risk among never smokers: https://pubmed.ncbi.nlm.nih.gov/28120396/
- PubMed meta-analysis of alcohol consumption and lung cancer risk: https://pubmed.ncbi.nlm.nih.gov/21427064/



